Services
News & Events

Make a smoke-free lifestyle your goal for 2018!
NANAIMO — If your New Year’s resolution is to quit smoking, Dr. Derek Poteryko can help.
Asthma is a long term disease (chronic) of the tubes that carry air into and out of our lungs (airways).
Learn about the signs and symptoms of asthma, how asthma is diagnosed, the triggers and causes of asthma, treatment and medication options.
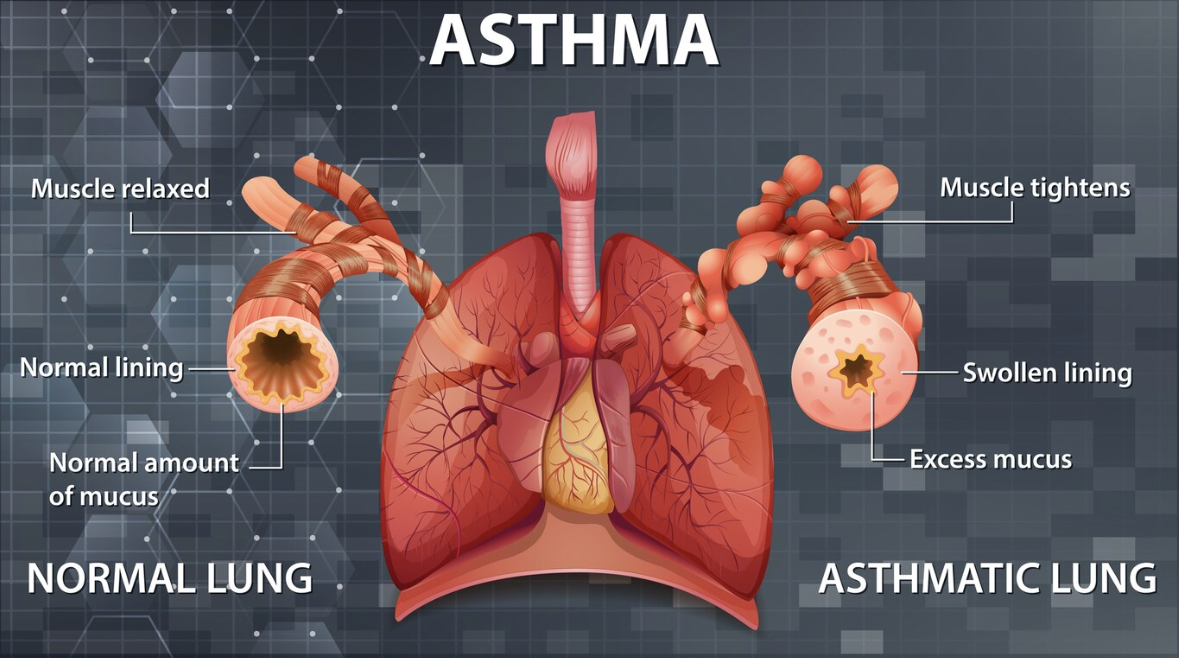
Asthma is a long term disease (chronic) of the tubes that carry air into and out of our lungs (airways). Asthma causes inflammation and narrowing of the airways which limits airflow and causes difficulty breathing. The airways of our lungs are surrounded by muscles and mucous glands, and normally these muscles are relaxed.
When a person with asthma encounters a trigger, the airways become inflamed, muscles tighten and the airway often fills with mucous. This makes breathing very difficult and may cause an asthma attack. A trigger is anything that irritates your airways. Triggers can be allergic such as dust, pollen and pet dander or non-allergic such as smoke, cold air and intense emotions.
It is estimated that 10.8% of Canadians have asthma. Asthma affects 3.8 million Canadians.
Six out of ten people with asthma do not have control of their asthma.
In Canada, asthma is the leading cause of missing school, and is the third leading cause of missing work.
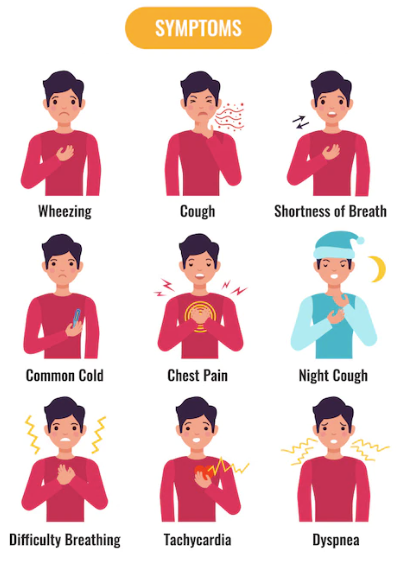
Asthma symptoms can be different for everyone and can vary over time. The most common symptoms include
Symptoms found on a physical exam, lung function testing and medical and family history support a diagnosis of asthma.
To confirm an asthma diagnosis, a breathing test (spirometry) is needed. This test occurs in a Pulmonary Function Lab where you breathe in and out through a mouthpiece attached to a machine that records the airflow. You take a big breath in and then blow out as hard as you can, then repeat this test after you inhale medication to open your airways. If there is a set increase in the airflow, asthma can be diagnosed.
When pulmonary function testing is not available, peak flows may be used to help establish a diagnosis.
Other tests that may be ordered are:

Once a Physician and Nurse Practitioner has confirmed you have asthma, you will have to learn about asthma control.
While there is currently no cure for asthma, with proper treatment and management you can live symptom-free. You are the one that knows how your asthma is affecting you so it is your responsibility to act when your asthma is not in good control. You must know your symptoms, triggers and medications well to help you live symptoms free.
The goal is to live symptom free.
Living symptoms free means having no daytime or nighttime symptoms, the ability to exercise without symptoms, no missed days of school, work or activities and having your breathing test/peak flow near personal best.
Poor asthma control may be due incorrect inhaler/medication use, incorrect inhaler technique, exposure to triggers or an incorrect diagnosis. Talk to your Healthcare provider if your asthma is not well controlled.
The Asthma Control Test (ACT) helps you and your healthcare provider know if your asthma is in control. This is a simple questionnaire available in numerous languages.
Triggers are any thing that can result in poorly controlled asthma, which can lead to an asthma attack. They can be allergic or non-allergic. It is very important you learn what your triggers are and try to avoid them. More exposure to triggers causes more inflammation which results in more symptoms and medication use.
Allergic triggers include pets, pollen, dust mites, and mold.
Non-allergic triggers include smoke, cold air, strong odours/chemicals, smog, infections (cold/flu), strong emotions, stress, thunderstorms and exercise.

Asthma is variable so understanding that your symptoms can vary throughout the year is important.
If you have asthma, your healthcare team will explain how to keep your asthma under control by avoiding your triggers, prescribe medications to lessen symptoms, show you how to use your medication and create an Asthma Action Plan.
An Asthma Action Plan is a personal plan on how to treat your asthma designed for you by your healthcare professional. Your Asthma Action Plan has your name, your medication names, and what your triggers are.
Green Zone
It works like a stop light, so if you are in the green zone, your asthma is well controlled and you are having no symptoms and your peak flows are 80-100% of your personal best.
Yellow Zone
When you start to have asthma symptoms, you move to the yellow zone and you will notice a drop in peak flows as well to 50-79% of your personal best. This is the zone you take action by increasing your medications as prescribed by your healthcare professional.
Red Zone
If you continue to have symptoms like being very short of breath, unable to do usual activities, your reliever does not help then it is time to go to emergency or call 911 as you are in the red zone.
Peak flowmeter is a device that you blow into as hard as you can into. When you blow into it, the device measures flow and the indicator states the highest flowrate. You will do this three times and record the highest number. This is a good indicator of how tight or swollen your airways are, and is included in your Asthma Action Plan.


Medications can be divided into three types; relievers, controllers/preventers and combinations of these two.
Relievers - they are short acting but fast to relax the muscles around the airway making it easier to breathe. These can also be called bronchodilators. They do not treat the cause of the asthma, which is inflammation. Using your reliever more than a couple times/week indicates poor asthma control.
Controllers/Preventers - they are longer lasting and work on the cause of the asthma, which is the inflammation/swelling. These can also be called corticosteroids. When taken regularly, they decrease the inflammation and mucous that block the airways. They do not work quickly, but they are the most important medication for treating asthma.
Combination relievers and preventers/controllers - this is one device containing two medications (bronchodilator and inhaled corticosteroid) that help decrease the cause of the symptoms, which is the inflammation in the airway, as well as the tight airway muscles.
There are many medications for asthma as seen in the "Asthma Medications" document below. It is important you discuss your medications with your healthcare professional.
Learn more about Asthma Medications.
With affective treatment and monitoring, you can live symptom free with your asthma. Please reach out to your healthcare provider with your questions and concerns.
Victoria - Royal Jubilee Hospital
250-370-8265
Central Island (Nanaimo, Oceanside)
250-739-5749
Toll free 1-877-734-4101
North Island (Comox, Campbell River, Mount Waddington)
250-331-8570
Toll Free 1-866-928-4988
Call 811 to talk to a nurse 24/7 and a pharmacist 5 - 9 p.m. daily. Translation interpreters are available in 144 languages.
Asthma Canada
BC Lung
Asthma Circle of Care Teaching Tool
Asthma Action Plan - Doctors of BC
Canadian Thoracic Society 2021 Guideline Update for Asthma
Global Initiative for Asthma

