Catch up on our recent research highlights and activities.
SPRING/SUMMER 2025
- New Research Policy
-
We're delighted to announce an important step forward in Island Health’s commitment to innovation, teaching and research: our first comprehensive policy for research.
Over the past 13 years, we have steadily expanded our research capacity, cultivating powerful partnerships, empowering clinical innovation and embedding evidence-informed practices into care. While we have long operated with standard procedures and guidelines, this new policy provides a unified, transparent framework for how research is supported, governed and seamlessly integrated throughout our entire health authority. The policy addresses key considerations such as:
- Working with First Nations, Métis and Inuit Peoples and partners to uphold Indigenous data governance and ensure that Island Health respects the First Nations principles of ownership, control, access, and possession, and the Métis principles of ownership, control, access, and stewardship.
- Fostering research culture and practices that respect and promote equity, diversity and inclusion.
- Ensuring that research is conducted to the highest scientific, ethical and professional standards.
- Fostering awareness of training requirements, other policies and research integrity supports.
We encourage you to explore the policy, consider its implications for your role, and connect with our team to share your questions, insights or ideas for collaboration. Together, we are fostering a culture where research inquiry, evidence and innovation can thrive.
- Announcing the Winners of the 2024-2025 KPMG Research Seed Grant Program
-
We're delighted to announce the successful applicants to the 2024-2025 KPMG Research Seed Grant Program. Funding for this competition has been generously provided by the Victoria Hospitals Foundation through support from the KPMG Foundation. Four grants of $12,500 were awarded this year to projects that:
- Align with Island Health’s priorities and goals to improve care and services in our communities and achieve our vision of “Excellent health and care for everyone, everywhere, every time."
- Engage people in research to gain experience, foster strong teams, and increase competitiveness for future funding opportunities.
Methadone for painful Chemotherapy-Induced Peripheral Neuropathy
Project Lead: Jessica Otte (Island Health)Chemotherapy-induced peripheral neuropathy (CIPN) is a common and painful side effect of chemotherapy, affecting up to 70% of cancer patients. The only recommended medication to relieve it is duloxetine, but its benefits are limited. Methadone, a drug often used to treat other types of nerve pain, has not yet been studied for CIPN. To see if methadone could be effective for CIPN, we are conducting a study comparing methadone to duloxetine in cancer patients who have painful CIPN with more than 12 weeks to live. This trial will last five weeks, with check-ins up to 24 weeks later. Participants will rate their pain, daily function, and quality of life through validated questionnaires. The goal is to determine whether methadone is effective in managing CIPN, a distressing condition with few treatment options.
iROBOT: Implementing Real-time Operational dashBOards for Trauma care
Project Lead: Christopher Picard (Island Health)This project aims to enhance trauma care coordination and data management using an advanced Artificial Intelligence (AI) system. Building on the current AI model developed by the Trauma and Island Health teams, we aim to expand the system's capabilities to identify all trauma cases, including those not resulting in transfers or admissions. This will enable real-time alerts for trauma services, improving support for patients in even the most remote areas. By enhancing decision-making, enabling faster responses, and providing comprehensive data, this project will improve patient outcomes, optimize resource allocation, and inform public health initiatives. It addresses an urgent need, applies existing knowledge innovatively, and ensures inclusivity in trauma care. This work is meaningful and valuable to stakeholders, offering a transformative approach to addressing a critical healthcare challenge.
Image-based storytelling for Indigenous informed consent
Project Lead: Paul Winston (Island Health)The informed consent process in healthcare often overlooks the unique cultural and communication needs of Indigenous Peoples, relying on written documents and complex medical terminology. Indigenous Peoples frequently encounter systemic barriers in healthcare communication, exacerbated by traditional consent processes that may feel intimidating or inaccessible. This project takes a transformative approach to informed consent using visual storytelling to create a culturally safe, trauma-informed, and engaging consent experience designed for Indigenous patients but transferrable to all. Visual narratives, grounded in Indigenous perspectives, will enable clearer communication, reduce intimidation, and foster trust between healthcare providers and Indigenous communities. To facilitate culturally safe informed consent, we will work with an Indigenous bioethicist and artist to create a video presentation that incorporates indigenous art and storytelling. By employing culturally safe, trauma-informed, and empowering narratives, we aim to provide a supportive healthcare experience that respects Indigenous identities and promotes clear, respectful communication.
An Online Tool for Parkinson Disease: Evaluating the Contribution to Care and Self-Advocacy
Project Leads: Larry Leung (UBC) and Amy Tran (Island Health)The research team has created an online tool to help educate individuals with Parkinson disease (PD) and care partners/caregivers about various PD medications and improve their ability to self-manage their medications. This project will assess the effectiveness of the tool by inviting individuals at all stages of PD to use the tool. They will be asked to share their thoughts and feedback, which will be used by the research team to improve the tool. Through a formal evaluation process that engages people with lived experience, the team will ensure that the online tool is informative and user-friendly, and empowers individuals with PD to self-advocate.
- Announcing the Winners of the 2024-2025 Health Research BC Health Equity Grants
-
We're delighted to announce the successful applicants to the 2024-2025 Health Research BC Health Equity Grant Program. Funding for this competition was generously provided by Health Research BC. Four grants of $12,500 were awarded this year to projects that:
- Advance health equity and eliminate health disparities by improving outcomes or access to health care and services for equity-deserving groups.
- Align with Island Health’s priorities and goals to improve care and services in our communities and achieve our vision of “Excellent health and care for everyone, everywhere, every time.”
- Engage people in research to gain experience, foster strong teams, and increase competitiveness for future funding opportunities.
Building a Compassionate Community: A Patient-Oriented Approach for Persons Seeking Medical Assistance in Dying
Project Lead: Caroline Variath (Island Health and Vancouver Island University)Island Health has the highest rate of Medical Assistance in Dying (MAiD) provision in BC. Recent research has highlighted gaps in our program’s support for equity-deserving populations seeking MAiD. MAiD legislation now allows provision for people whose natural death is not foreseeable; however, they do not meet criteria for palliative or end-of-life care. Rising rates of substance use, mental health disorders, and homelessness further underscore the need for compassionate, supportive care for those considering MAiD. Many non-profit community organizations that provide health and social services for equity-deserving groups lack awareness about MAiD and its processes, limiting their ability to offer informed support.
Dr. Variath and her team have received a Health Research BC Health Equity Grant to address these gaps and foster collaboration between Island Health's MAiD program, people with lived or living experiences, and local community support organizations. The primary goals are: 1) to explore and strengthen community-based supports available for equity-deserving populations seeking MAiD on Vancouver Island and 2) to enhance awareness and understanding of MAiD among community support organizations. This project will establish a strong foundation for developing an integrated Compassionate Community approach that offers wrap-around support to persons seeking MAiD and their families.
Developing therapeutic groups using tabletop roleplaying games (TTRPGs) in tertiary pediatric mental health
Project Leads: Sonya White, Ryan Wong, and Jennifer Harcus (Island Health)
Youth with complex mental health and neurodevelopmental differences benefit from diverse opportunities to practice using coping strategies. These youth also benefit from therapeutic opportunities that leverage internal motivation to participate, so it’s important for them to have fun in therapy. It’s also important for these youth to trial the use of strategies in peer-based environments that offer flexible levels of instruction and support.
Current service formats do not meet these needs, so Sonya’s team will evaluate the use of tabletop roleplaying games (TTRPGs) for therapeutic purposes in outpatient youth mental health settings. TTRPGs are saturated with humour, risk-taking, and creativity. TTRPGs bring players together to solve problems. The problems evolve and are shaped based on participant choices and interests, and solving the problems is an inherently social task. This means that TTRPGs manifest many of the same social demands and challenges that youth encounter at home and at school. In this sense, TTRPGs are a natural vehicle for bridging the gap between outpatient treatment and real-life function.
Together with youth and their families and carers, the team will explore TTRPGs as a natural creative space in which youth can learn to self-monitor, self-regulate, and advocate for themselves.
Exploring Safe and Affirming care through the lived experiences of 2S/LGBTQIA+ people
Project Leads: Ingrid Handlovsky and Allie Slemon (University of Victoria); Chandra Berkan-Hozempa (Island Health)
Two-Spirit, lesbian, gay, bisexual, trans, queer, intersex, and asexual (2SLGBTQIA+) people experience discrimination in their day-to-day lives that greatly contributes to poorer health outcomes. Health service settings are common sites of discrimination for 2SLGBTQIA+ people, who often feel unsafe and fear mistreatment, which leads to reticence to access essential health services altogether.
Care approaches within health care settings must be adapted and informed to better meet the unique needs of 2S/LGBTQIA+ people to ensure equitable and safe care. Emerging research suggests that affirming care that centres respect, cultural competency, identity recognition, and person-centred practices can foster trust, and improve communication and overall well-being.
Building on these insights, this research adopts a strengths-based approach to explore how 2S/LGBTQIA+ individuals and healthcare providers conceptualize and experience safe and affirming care in hospital settings. By shifting attention from discrimination to affirmation, this work seeks to identify the relational, cultural, and structural factors that contribute to safety, dignity, and belonging in healthcare.
A Pharmacist's Role in a Parkinson's and Movement Disorders Clinic: Evaluating the Impact on Workflow and Patient Experience
Project Leads: Larry Leung (UBC) and Amy Tran (Island Health)Parkinson disease (PD) is a chronic and progressive neurodegenerative condition. The wait time to see a provider at the Parkinson's and Movement Disorders Clinic at the Royal Jubilee Hospital in Victoria, BC is 24 months. Because PD is progressive, changing symptoms can be difficult to manage in between appointments, leaving individuals feeling unsupported and adjusting their medications without guidance.
To address this need, this research project will evaluate the impact of integrating of a pharmacist into the interdisciplinary team at the Parkinson's and Movement Disorders Clinic at the Royal Jubilee Hospital in Victoria. A committee of individuals with Parkinson disease (PD) and care partners/caregivers will be fully engaged throughout the project to help ensure that the integration of the pharmacist into clinic operations will effectively address the health needs of the PD community.
First, a needs assessment will be conducted so patients and team members of the clinic can provide their input and feedback. The pilot phase will then implement the integration of the pharmacist on the team. Finally, the research team will evaluate the impact on workflow and efficiency from both the patients’ and clinic staff perspectives, enabling them to identify effective and meaningful solutions.
- Must-Read: Our Latest Research in Review (2024-25)
-

The latest Research in Review highlights the breadth and impact of research across our region, showcasing how local inquiry is improving outcomes, advancing health equity, and enhancing service delivery.
Featuring:
- Bridging Indigenous and Western Medicines
- Advancing Treatment for Dementia
- Supporting Patients before Life-Changing Laryngectomies
- Co-op Students for Cryoneurolysis
- Impact of Clinical Research on Critical Care
- Research by the Numbers
Read the new Research in Review!
FALL 2024
- Introducing Dr. Amy Salmon: Conconi Family Foundation Distinguished Scholar in Seniors Care
-

With the support of the Conconi Family Foundation, Providence Living, the Centre for Advancing Health Outcomes, the Comox Valley Healthcare Foundation, Nanaimo & District Hospital Foundation, the Eldercare Foundation and Island Health, Dr. Amy Salmon has been named the inaugural Conconi Family Foundation Distinguished Scholar in Seniors Care.
“The purpose of the Scholar is to ask the questions that matter and find the answers needed to create systems that provide better seniors’ care now and for generations to come,” says Dr. Salmon.
Dr. Salmon is a Clinical Associate Professor in UBC’s School of Population and Public Health and has long been recognized for her leadership in participatory, community-engaged research and developmental evaluation. As Scholar, she will be embedded in the health system to support adoption of new evidence and innovation across the province, starting on the North Island. Dr. Salmon is currently a resident of the Comox Valley.
“It’s really exciting to see everyone coming together with a real willingness to do things differently, to do things better,” says Dr. Salmon. “Capturing that and supporting that work through our research is something I’m excited about.”
Funds will support dedicated leadership by Dr. Salmon and the work of a full team in seniors’ care researchers from January 2024 to January 2034.
SUMMER 2024
- Announcing the Comox Valley Dementia Care Pilot Grant Recipients in Patient-Oriented Research
-
Congratulations to the three teams who have been awarded Comox Valley Dementia Care Pilot Grants in Patient-Oriented Research (POR)!
POR is about engaging people with lived and living experiences throughout the research process to ensure that studies focus on patient-identified priorities, leading to better outcomes.
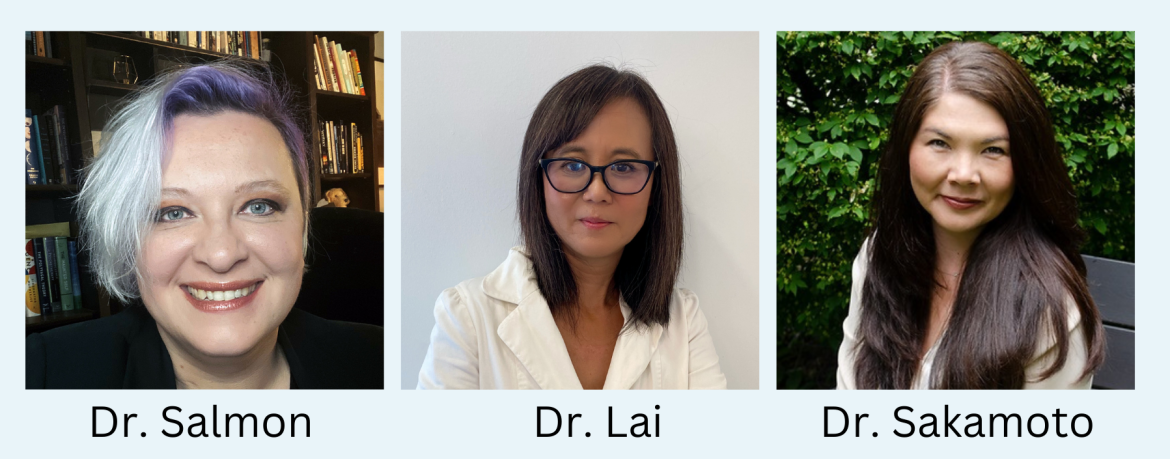
Mapping the Comox Valley’s Integrated Community Care Ecosystem for Older Adults living with Dementia (Dr. Amy Salmon)
Dr. Salmon is a Distinguished Scholar in Seniors Health and Community Care and an associate director of the Centre for Advancing Health Outcomes. She has recently moved to the Comox Valley. Her team will focus on mapping the region's integrated community care ecosystem for older adults living with dementia. With this knowledge, Dr. Salmon's team will co-develop an intervention with older adults living with dementia and seek national grant funding to support the work.
Staying at home longer with dementia: Co-developing tools with informal caregivers for building a learning health community (Dr. Claudia Lai)
Dr. Lai is a clinician-researcher and assistant professor of Health Informatics at the University of Victoria. The POR team will co-develop tools with informal caregivers to build a learning health community in the Comox Valley. An advisory group with lived experience of dementia, that understands the care and support needs of older adults living with dementia, will help guide the research.
Working Together: A Dementia-Friendly Community for the Comox Valley (Dr. Mariko Sakamoto)
Dr. Sakamoto is a nurse researcher and assistant professor at the School of Nursing at the University of Victoria. Her POR team will work to build a dementia-friendly community for the Comox Valley. By engaging people with lived experience of dementia, and working with members of the Comox Valley community, the team will raise awareness and a better understanding of dementia and the needs of people affected by the condition, as well as address and decrease dementia-related stigma.
Congratulations Claudia, Mariko, Amy and teams! We are excited to work with you!
Thank you to the Comox Valley Community Foundation who made these grants possible through a generous contribution from the Robert and Florence Filberg Fund, held at the Vancouver Foundation and facilitated by the Comox Valley Healthcare Foundation.
SPRING 2024
- Health Equity and KPMG Foundation Research Seed Grants Awarded
-
We're delighted to announce the successful applicants to Island Health's 2023-2024 research seed grant competition. This competition funds health research projects that:
- Align with Island Health’s priorities and goals to improve care and services in our communities, and achieve our vision of “Excellent health and care for everyone, everywhere, every time.”
- Engage people in research to gain experience, foster strong teams, and increase competitiveness for future funding opportunities.
This year, 4 general seed grants of $12,500 each were awarded, as well as 2 seed grants of $12,500 each to support health equity projects in the Greater Victoria area. These projects will to advance health equity and eliminate health disparities by improving outcomes or access to health care and services for equity-deserving groups.
Funding for this competition has been generously provided by the Victoria Hospitals Foundation through support from the KPMG Foundation and the Victoria Foundation.
Health Equity Grants
Preventing seclusion for young adults in inpatient mental health
Allie Slemon (University of Victoria) and Tasha Mckelvey (Island Health)75% of mental illnesses first present by age 24. However, mental health inpatient admissions are traumatizing for many young adults, especially when they face seclusion: confinement in an isolated locked room, usually to manage acute risk of violence or harms. This spring, Royal Jubilee Hospital opened a Young Adult Mental Health Inpatient Unit to support young adults (17 to 26) who are experiencing severe mental health challenges. This project brings together researchers and Island Health leaders with peers and young people who have lived experience of seclusion. They’ll identify strategies for preventing seclusion while ensuring that any changes are equitable and grounded in the voices of those most affected.
Integrating Mental Health and Substance Use Supports for Residents in Long-term Care
Amy Salmon (University of British Columbia) and Amanda Leddy (Island Health)Long-term care (LTC) provides 24-hour care, accommodation, and hospitality to adults with complex medical and cognitive health issues. While most LTC residents have traditionally been older adults living with complex health conditions such as dementia and frailty, a growing number of younger people with developmental, brain injury, and mental health and substance use needs are living in or waitlisted for LTC homes. The Summit, a LTC home in Victoria, has developed a specialized care unit for people who do not fit the traditional LTC resident profile. The unit is currently home to 32 people, many of whom have a history of precarious housing or homelessness and complex mental health and substance use issues. Through this innovative care model, residents can access services rarely or never available in other LTC homes, such as harm reduction supplies, prescribed safer supply, and opioid agonist therapy. This project will engage and explore the perspectives of those residents, enhancing services to better meet their needs and improve their experience.
KPMG Foundation Research Seed Grants
Safety Interventions: Are they helping healthcare workers feel safer?
Frances Jorgensen (Royal Roads University) and Michael Morrison (Island Health)Workplace violence is on the rise in healthcare, and has serious consequences for employees, patients, and our communities. Emerging research also suggests that equity-deserving employees are more often the target of workplace violence and may suffer more enduring negative consequences. Many ways to prevent workplace violence have been proposed and implemented, but we don’t know how healthcare employees actually experience these interventions, or whether they feel safer as a result. This project will ask hospital employees whether violence prevention in their workplace has increased their sense of safety, and how it could be more effective. The research team aims to develop practical ways to improve violence prevention, enhancing employee safety and reducing risk.
Recharging the Charge Nurse: developing the next generation of nurse leaders
Lenora Marcellus (University of Victoria) and Kent Soltys (Island Health)Charge nurses, or unit leaders, are critical to the successful operation of clinical care units. They coordinate and mobilize resources, respond rapidly to changing demands and conditions, create a positive work culture, and are accountable for patient safety and quality care. Within Island Health, the role has usually been given to the most senior or expert nurse on shift, yet many are now retiring. In Island Health’s annual survey of new registered nurse graduates, 60% reported being appointed as charge nurses within their first 6 months, yet many lack access to training and support specific to this complex point-of-care leadership role. This project aims to describe the experiences of Island Health charge nurses, how they were prepared for the role, the challenges they experienced, and how they developed as leaders. The results will contribute to improving satisfaction and retention, and creating an initial foundation for and interest in nursing leadership development.
Catalyzing action to reduce preterm birth among Indigenous people in BC
Jennifer Murray (University of British Columbia) and Shannon Waters (Island Health)Worldwide and in Canada, Indigenous women face an increased risk of adverse birth outcomes, including preterm birth. Preterm birth is any birth before 37 weeks of gestation, and has long-lasting health impacts on the infant, parents, and family. These disparities are linked to the impacts of historical and ongoing colonization that have severely disrupted Indigenous people's lives, culture, and the intergenerational transfer of knowledge. An ongoing community-based study has found that the rate of preterm birth is three times higher for Quw'utsun (Cowichan Tribes) community members than for non-First Nations births. The goal of this project is to reduce the risk of preterm birth by catalyzing health system change and fostering strong, healthy, and thriving Indigenous communities in Quw'utsun, across Vancouver Island, and throughout BC. To achieve this goal, the team will prepare a policy brief and engage in deliberative dialogue with policymakers and health service leaders.
Improving quality of life and reducing pain for children with spasticity
Dr. Paul WinstonSpasticity causes muscle stiffness, pain, and disability for millions of adults and children worldwide. It affects up to 70% of children with cerebral palsy, as well those have experienced strokes, spinal cord injuries, or severe traumatic brain injuries. Spasticity can cause painful and deformed joints, and may result in disability; as they grow, children either need constant injections with botulinum toxin, or major surgeries. This research project will document the impact of an innovative treatment for spasticity in children: cryoneurolysis or nerve-freezing is a quick, long-lasting, and cost-effective procedure. The study will measure mobility, function, independence, pain, and quality of life following cryoneurolysis. Learn more about cryoneurolysis for spasticity in this short video.
WINTER 2024
- New Research in Review: Read the 2023 Annual Report
-
In the 2023 calendar year, we continued to support our vision of excellent health and care for everyone, everywhere, every time. Thriving research collaborations are changing lives and improving services by:
- preventing vascular risk
- reducing migraine pain through a clinical trial
- preventing injury in community healthcare workers
- co-creating a response to the toxic drug poisoning crisis
- engaging community to improve dementia care in the Comox Valley
- empowering people through better data management
SUMMER 2023
- Engaging Community to Spark Aging, Dementia, and Long-Term Care Research in the Comox Valley
-
July 2023

The Comox Valley Community Foundation has awarded Island Health $130,000 from the Robert and Florence Filberg Medical Research Grant to engage community in improving care and services for an aging population.
The grant was facilitated by the Comox Valley Healthcare Foundation; President Bill Anglin notes that “aging well and growing old are on the minds of many in our community. The Comox Valley Healthcare Foundation, working alongside Island Health, is placing a spotlight directly on aging well and growing old. We are grateful for the generous funding provided by the Comox Valley Community Foundation.”
Some of the grant will support a local research priority-setting workshop in September 2023. The workshop will bring together patients--including family members, caregivers and friends--researchers, clinicians and healthcare decision-makers to identify the community’s top priorities around aging well, dementia, and long-term care. “We’re thrilled that the Comox Valley Community Foundation and the Comox Valley Healthcare Foundation are supporting research collaborations with patients and communities," says Cindy Trytten, Director of Research.
The workshop’s patient-oriented approach engages people with lived experience as equal partners through the whole research process, from setting priorities to ensuring that the results will improve outcomes. For Max Jajszczok, Executive Director, Rural and Remote Strategy, “The Filberg Medical Research Grant will empower the people who receive our services to identify their research priorities for aging and dementia care by bringing them together with researchers, clinicians, and health system leaders to improve experience and outcomes.”- Read the report on what we heard at the workshop.
Following the workshop, the majority of the grant will be distributed through a grant competition to fund research projects and fellowships that address the top priorities. These projects will have a tangible local impact, paving the way for participation in studies, fostering more research opportunities, and shaping a brighter future for aging and dementia care.
Learn More
- Comox Valley Community Foundation funds aging and dementia research (Comox Valley Record)
- Patient-oriented research support at Island Health
Interested in contributing or participating? Connect with us!
- Uta Sboto-Frankenstein, Patient-Oriented Research Navigator, Mid and North Island (uta.sbotofrankenstein@islandhealth.ca)
SPRING 2023
- Congratulations to the latest crop of research seed grant winners!
-
June 2023
The results are in! Congratulations to the three successful teams, who will receive $7,500 each to support the following projects:
- Improving frailty care in Cowichan: Lina Al-Sakran (evaluation consultant, Cowichan Health & Wellness Plan) will take a patient-centred approach to improve community care and services for people living with frailty in the Cowichan Valley. This study aims to understand the needs of Cowichan Valley seniors, and identify opportunities to improve services that will support older adults to live independently in the community.
- Supporting patients before life-changing surgery: Meara Brown (speech language pathologist) will map the care journeys and counselling experiences of patients who have total laryngectomies: the complete surgical removal of the voice box. Drawing on the help and expertise of the laryngectomy community, this is a first step towards building a counselling framework to better support patients before a life-changing surgery with profound social, economic, and health consequences.
- Engaging Indigenous youth to measure connections to culture and land: Jennifer MacKenzie (regional youth MHSU nurse clinician & youth intensive case management team coordinator), Andrea Mellor (UVic) and Cecelia Benoit (UVic) will engage with Indigenous communities in Victoria and Cowichan to evaluate a meaningful way of measuring connections to culture and land for Indigenous youth who access mental health and substance use services. Cultural interventions take a whole-person and strengths-based approach, and measure hope, belonging, purpose, and meaning.

From left: Lina Al-Sakran, Meara Brown, and Jennifer MacKenzie
Meaningful Review, Meaningful Projects
For the first time in an Island Health grant competition, the application review process included patient and community partners alongside clinical and academic reviewers. All reviewers were invited to evaluate all applications to the competition. Their scores and feedback were weighted equally, and combined to determine which projects would receive funding. Designing a balanced and meaningful review process that brings together many perspectives is one way to make sure we're funding research that matters to the communities we serve. It also helps to ensure that the funded projects are designed and conducted with patients, families, and communities in mind as equal partners.
The patient partners were supported throughout the review process by Island Health’s Leader for Patient and Public Research Engagement. Patient partners include anyone directly affected by a health condition, illness, or health system issue: family members, loved ones, and care givers as well as patients. There are lots of ways to get involved in research beyond participating as a study subject. Whether you're interested in joining a research team, helping set priorities for future research, reviewing grant applications, or contributing to events and education, your experience provides a unique and valuable perspective.- Complete this brief survey and we'll be in touch when we have a local opportunity that fits your interests.
Emerging Stronger
Funding for this competition was made available through the Victoria Hospitals Foundation’s Emerge Stronger campaign. This $10 million campaign provided $500,000 to fund research projects that support the provision and delivery of care in the South Island and/or Island-wide.
We are grateful to the Victoria Hospitals Foundation and their very generous donors for supporting health research on Vancouver Island. To donate or to learn more about these projects and others, visit the Foundation's website.
- Improving frailty care in Cowichan: Lina Al-Sakran (evaluation consultant, Cowichan Health & Wellness Plan) will take a patient-centred approach to improve community care and services for people living with frailty in the Cowichan Valley. This study aims to understand the needs of Cowichan Valley seniors, and identify opportunities to improve services that will support older adults to live independently in the community.
- New Research in Review Highlights Collaborations & Impact
-
April 2023
Curious about what we've been up to recently? Check out our Research in Review, a report that highlights just some of the inspiring researchers at Island Health and the people whose lives they impact in so many positive ways. Research is all about collaboration, relationships, learning, and inquiry; thank you to those who support what we do!
Read our Research in Review
- REDCap Data Management: Celebrating 10 Years + 1,000 Projects at Island Health
-
March 2023
REDCap (Research Electronic Data CAPture) is a powerful data management tool that’s advancing health services management, quality improvement, innovation, and research at Island Health and across BC.
On March 22, we reached a major milestone: 1,000 REDCap projects have been created at Island Health since its launch in 2014!
- Check out this infographic celebrating 10 years of REDCap at Island Health
- Get the details on its evolution at Island Health in this report.
The 1,000 Project: Snapshot
Who requested the 1,000th project? Aimee Falkenberg, a forensic nurse examiner and clinical coordinator for the Nanaimo Forensic Nurse Examiner Program (Central and North Island). Learn more about Forensic Nursing Services at Island Health.

How will Aimee use the project? Aimee and her team will use REDCap to collect statistical data for the forensic nursing program. This will allow them to increase their skillset and educate forensic nurse examiners; it will also shed light on the increasing levels of intentional violence and injuries they’re seeing. Forensic nurses are on call 24/7 and 365 days of the year. They see survivors of intimate partner violence, intentional relational violence, family violence, sexual exploitation and sexual assault across the lifespan, all genders up to seven days post incident.
What’s the impact? Aimee says that “having data to show what types of injuries we are seeing and the significance of those injuries to the health and wellbeing of survivors will help us develop interventions and research projects that will directly impact care outcomes. I am excited to start this project, to see the benefits of the data collection and to make deeper and greater impacts for survivors of intentional traumatic violence.”
Why did Aimee choose REDCap? It came with a strong recommendation: “Using REDCap for data collection was a very easy decision to make. Trauma Services is using REDCap for a large trauma project and Darren Chan (trauma coordinator for Central and North Island) said it was seamless to use and crucial to the work they do.” says Aimee.
Learn More about REDCap
- Island Health employees can request a REDCap project estimate.
- Researchers at other institutions within British Columbia may be eligible to access REDCap through PopDataBC. Learn more.
- Get inspired by these innovative REDCap projects at Island Health.
WINTER 2023
- New Research Network to Improve Care for Acquired Brain Injury
-
January 2023
Vancouver Island University (VIU) researcher Dr. Sandy Shultz and Island Health's Aimee Falkenberg (clinical coordinator for the Forensic Nurse Examiner program, Central and North Island) are leading a patient-oriented research team to improve care for survivors of intimate partner violence who have experienced a brain injury.
There isn't a lot of research on Acquired Brain Injury (ABI) as a result of Intimate Partner Violence (IPV), which can be difficult to diagnose because there is no current standard for screening. ABIs can be misidentified as emotional distress or struggles with mental health or substance use, and symptoms may not occur immediately after an assault. Targeted assessment tools are urgently needed.
In December, a group of clinicians, researchers, community organizations, and people with lived and living experience of ABI/IPV gathered in Nanaimo to establish a patient-oriented research network.

Supported by members of Island Health's Research Department and funded by a Michael Smith Health Research BC grant, the event built on a longstanding collaboration between the Nanaimo Brain Injury Society, academic & community partners, and Island Health.
Forensic nurses and people with lived experience underscored the lack of assessment tools and treatment protocols for ABI/IPV survivors, and identified priorities and next steps for collaboration. Dr. Shultz presented his novel blood-biomarker research protocol developed to enable rapid and accurate diagnosis of ABI/IPV. Attendees reviewed the protocol to optimize its implementation at Island Health and will support the recruitment of ABI/IPV survivors to test the blood biomarker later this year.
Learn More:
- Resources and Support for Acquired Brain Injury
- Explanations of IPV in BC
- Intimate Partner Violence & Acquired Brain Injury (Evidence Synthesis)
- Find out about patient-oriented research
Get Involved:
- Connect with Uta.SbotoFrankenstein@islandhealth.ca to learn more about this project.
- Ask Taylor.Hainstock@islandhealth.ca about engaging patients and families as equal partners in research.
