January is Alzheimer’s Awareness Month, a time to learn more about dementia and its impact on patients, families and caregivers. Island Health’s primary care memory clinics support patients and families concerned about memory loss.
Established in 2021 in Victoria and Nanaimo and based on Dr. Linda Lee’s nationally recognized MINT (multispeciality, interprofessional team) memory clinic model, the Island Health memory clinics offer services in partnership with the Alzheimer’s Society.
“Our goal is early intervention where we see patients experiencing memory issues as quickly as possible in order to provide a diagnosis and connect patients and families with the supports they need, including community services,” says Michael Pojol, Manager, Victoria Primary Care Memory Clinic. “We want to support people of all ages with early diagnosis and treatment and ensure they receive the right care at the right time and in the right place.”
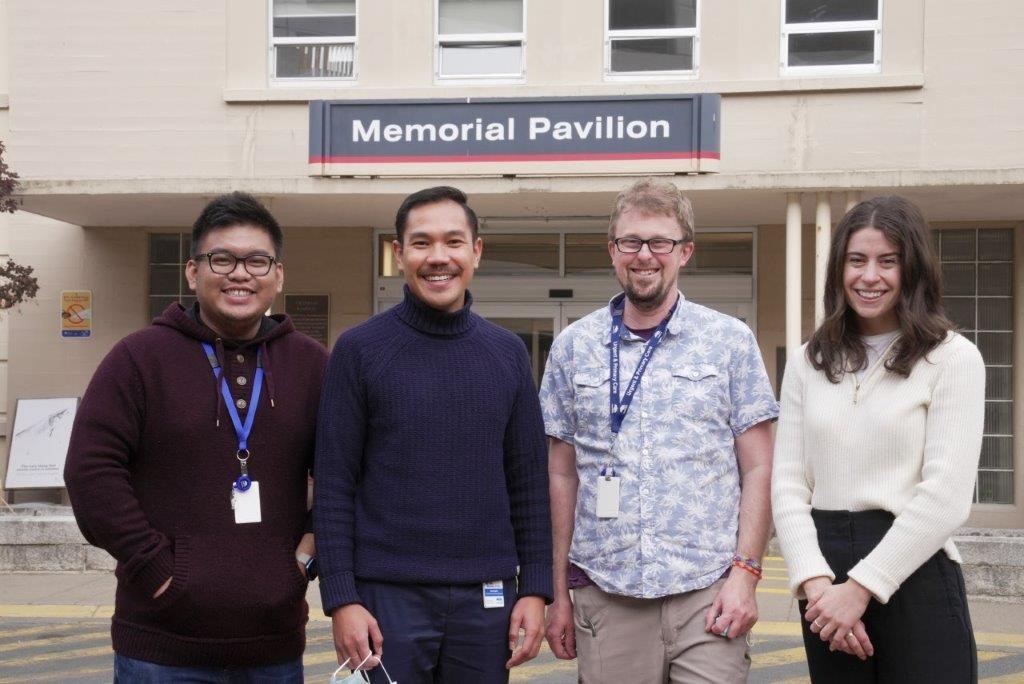
Victoria Memory Clinic Team
Not all symptoms of memory loss are caused by dementia. In some cases, memory loss can be caused by other issues, and once these are resolved, the issue with memory loss is resolved, too.
“There are times where our intensive assessment can pinpoint other conditions that aren’t dementia,” says Julia Kuhn, a registered nurse and leader within the Nanaimo Primary Care Memory Clinic. “Sometimes medication will impact cognitive function. At other times, it may be an undiagnosed condition. The key really is early diagnosis and from there, we can develop a treatment plan.”
Eligible people can be referred to the memory clinics by their primary care provider or through urgent and primary care centres and walk-in clinics.
“The services we offer are timely, comprehensive, compassionate and holistic,” says Dr. Valerie Ehasoo, a physician at the Victoria Primary Care Memory Clinic. “We know that the services we provide help to improve quality of life for our patients and their caregivers, reduce emergency room visits, decrease hospital admissions and defer or delay the need for an individual to move into a long-term care home. This creates significant benefits for our patients, their families, and the care providers and community partners who work collaboratively on this multidisciplinary team.”
During initial appointments, patients are encouraged to attend with loved ones or caregivers. A memory clinic team, including a family physician, social worker, registered nurse, occupational therapist, medical office assistant and a representative from the Alzheimer’s Society, meets with the patient and family member or caregiver and talks with them about their experience with memory concerns and cognitive deficits. The Nanaimo memory clinic team also includes a pharmacist.
“We discuss activities of daily living, sleep patterns, their mood and family medical history,” says Scott Mackay, a social worker at the Victoria memory clinic. “Then, the Alzheimer’s representative and I meet with the family caregiver to learn about their experiences with their family member, while the patient meets separately with our nurse and occupational therapist for formal cognitive testing and a physical assessment.”
“Our Nanaimo Alzheimer’s Society representative, Jane Hope, is an invaluable resource and member of our team,” says Kuhn. “She often guides clients and loved ones into the exam room, making them feel comfortable before the assessment, which can take a couple of hours. She’s there to provide advice, guidance and connections to community resources during what can be an overwhelming time for people who may receive a dementia diagnosis.”
Nanaimo Memory Clinic Team
During the initial appointment, the multidisciplinary team gathers to discuss the patient’s test results and often confirms a diagnosis. The patient and family caregiver then meet with the physician to discuss the diagnosis, ask questions and receive recommendations for medications, necessary referrals to specialists for further investigation or clarification, and links to community supports. Between follow-up appointments, patients and caregivers are encouraged to reach out to clinic staff with questions and concerns.
“It’s important to offer them support by helping them to figure out ‘where do I go from here?’,” says Mackay.
“We connect clients who are living with dementia and their caregivers to First Link® dementia support services, education and information at any stage of the disease,” says Glenda Kopperson, Alzheimer Society of B.C.’s First Link® Support and Education Coordinator. “The memory clinics ensure that clients receive support and information relevant to their situation. Many have commented that it is a relief to find information and support at the initial meeting and to learn that they are not alone.”
Lisa Kochem’s 78-year-old mother is a recent patient of the Victoria Primary Care Memory Clinic. She was referred to the clinic in October 2021 after experiencing gradual memory decline over the past several years.
“Being referred to the memory clinic provides a baseline to start from. You have to start somewhere, and they are there to help you to navigate the process,” says Kochems. “You receive such a wealth of information, and the help is there. It’s been very overwhelming, and, even though they can’t cure my mom’s disease, they have been able to help slow the progression and make things a little less stressful.”
“It’s really hard, but I know I can call them anytime, ask questions and get advice,” she says.
Currently, the Victoria clinic, located at Memorial Pavilion on the Royal Jubilee Hospital campus, is open two days per week to residents of downtown Victoria, Vic West, James Bay, Oaklands and Gordon Head, while the primary care memory clinic at the Nanaimo Health Unit is open one day per week for residents of Nanaimo.
“This role is very satisfying. I truly value my time with the memory clinic,” says Mackay. “I’m honoured to know that our team has played a role in supporting a patient and their loved ones to receive a formal diagnosis, link them to resources and get the supports in place to help them maintain where they are at for as long as possible.”
“It is important for people to know that they aren’t alone following a dementia diagnosis. Our goal is to make those connections for patients and families and ensure they feel well-supported during this difficult journey,” says Kuhn.
According to the Alzheimer’s Society of Canada, there are more than half a million Canadians currently living with dementia with that number projected to rise to nearly one million people by 2030.